Managing mastitis
Updated April 10th, 2024
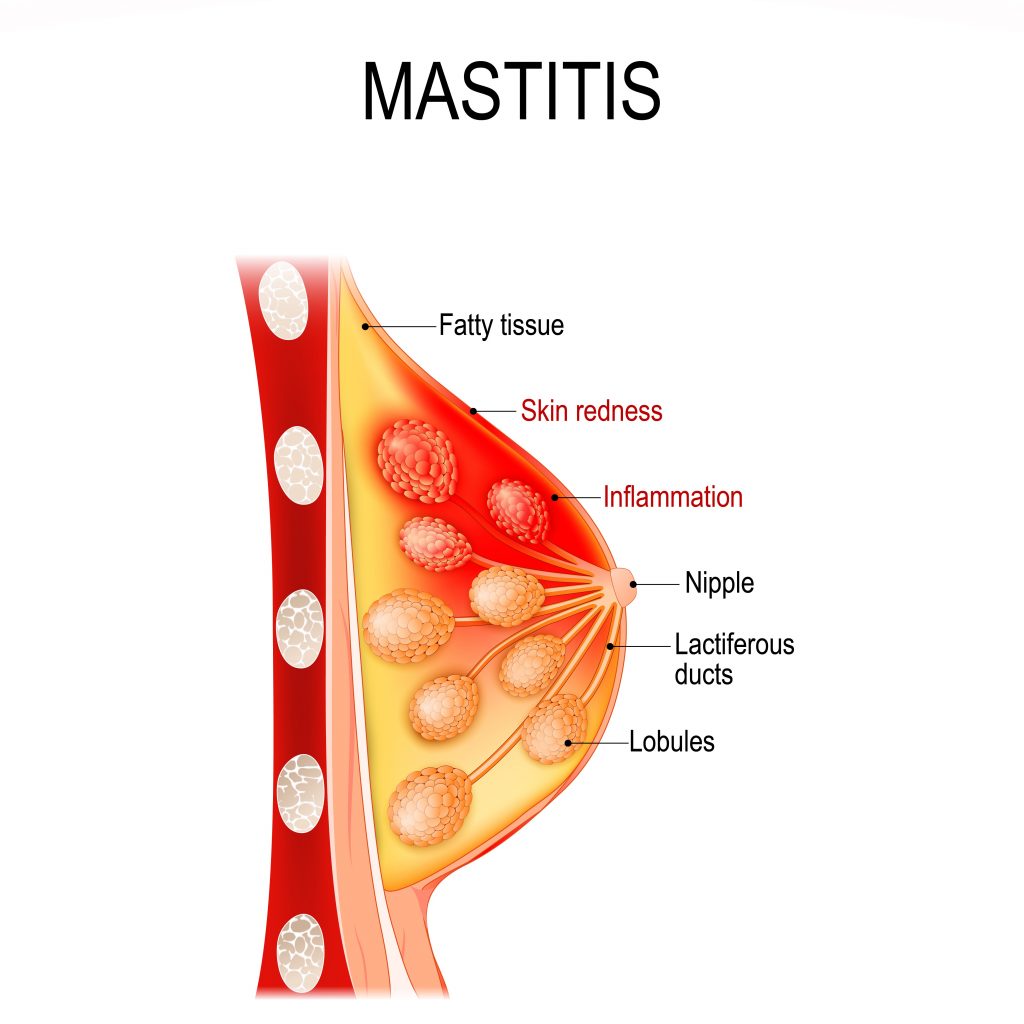
Mastitis is painful inflammation in the breast tissue that can affect parents who breast/chest feed or exclusively pump. Mastitis can cause pain, swelling, warmth and redness on your breast and can make you feel run down and tired. Parents can continue to breastfeed their babies while mastitis is healing.
What are the symptoms of mastitis?
- Red, warm or swollen breast
- Tender lump in your breast
- Nipple bleb or milk blister
- Flu-like symptoms like fever (greater than 38°C), chills, body aches
What causes mastitis?
Mastitis is most commonly caused by overactive milk production (hyperlactation) through over-pumping or medications used to increase breastmilk supply. Oversupply of milk causes the breast tissue to put pressure on the milk ducts, and may cause plugged ducts, engorgement and inflammation. Skipped feeds, poor latch, a poorly fitting breast pump flange or recent use of antibiotics can also lead to mastitis.
In some cases, mastitis inflammation can lead to infection (bacterial mastitis) or an abscess (a collection of fluid and pus under the skin).
What can I do to ease mastitis?
What to do |
What to avoid |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
Hot parent tips:
- Ask your family and friends for help so you can rest.
- If the recommendations above don’t improve your mastitis and you develop flu-like symptoms that last more than 24 hours, call your health care provider.
“I always heard you are supposed to empty your breasts to help with mastitis…..have things changed?”
The new recommendation is: If you are separated from your baby or are exclusively pumping, aim to produce only the amount of milk your baby needs and not more. If you need help breastfeeding your baby, reach out to your public health nurse, knowledge keeper, midwife or health care provider.
In the past, it was thought that “emptying your breasts” more often would treat the symptoms of oversupply. New research (as of 2022) shows that this actually makes engorgement worse. Emptying your breasts more often (by pumping or feeding) will only lead to more milk production and more inflammation.
How can I prevent mastitis?
- Breastfeed your baby based on their hunger cues. Make sure your baby has a good latch and position.
- Get help early if you have concerns about breastfeeding. Check out our Breastfeeding Resources page.
- Pump breastmilk only if you have to be away from your baby or you plan to give a bottle instead of feeding at the breast.
- If you are exclusively pumping, pump only the amount of milk your baby needs and not more.
- When using a breast pump, use the most comfortable pressure setting and pump for 10-15 minutes. Make sure your breast pump flange is the right size for you.
- Wear are good-fitting bra without underwires. It shouldn’t be tight or restrictive.
Why do my breasts feel like they are going to explode?
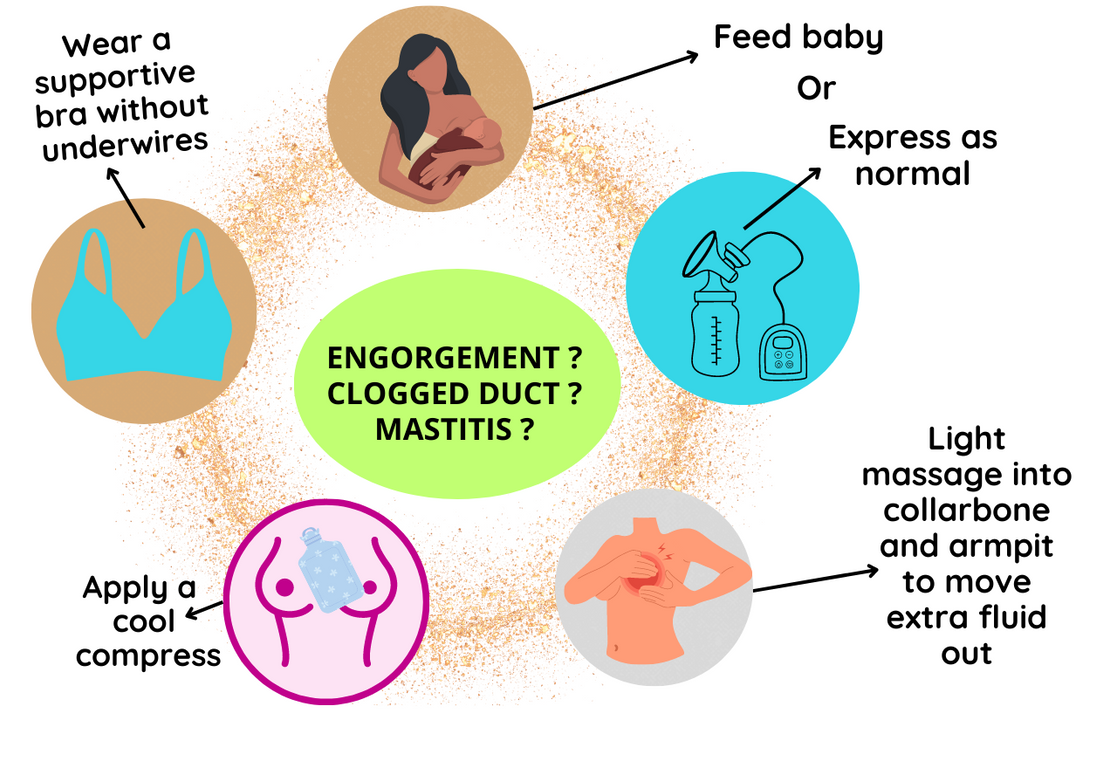
- In the early days of breastfeeding, it is common for breasts to swell up with milk. They may feel full, heavy and sore. This is called engorgement. You may mistake it for mastitis.
- Engorgement can also happen later on if feedings are missed.
- The good news is, engorgement generally only lasts a couple of days.
- To learn more on how to manage engorgement, click here.
Resources:
- Printer friendly infographic: mastitis, engorgement, plugged management options April 2023
References:
- Academy of Breastfeeding Medicine Clinical Protocol #36: The Mastitis Spectrum, Revised 2022
- Baby’s Best Chance: 7th Edition pages 118-119